What is Cardiometabolic Health?
Cardiometabolic health refers to the overall well-being of your cardiovascular system (your heart and blood vessels) and metabolic system (how your body breaks down food to create energy). Maintaining good cardiometabolic health is vital for a longer, healthier life.
Understanding Cardiometabolic Health
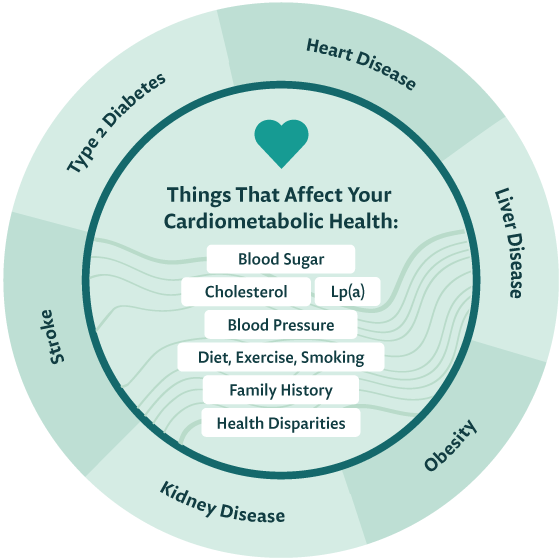
Here’s the bigger picture: obesity, type 2 diabetes, chronic kidney disease, and heart disease are all connected. Doctors know that having one of these conditions greatly increases your chances of getting another. This is because these diseases share common risk factors — health conditions influenced by your lifestyle, your age, and your family history.
Rather than focusing only on the heart, doctors are looking at managing the common risk factors like your blood pressure, your blood sugar, your cholesterol, as well as lifestyle choices and genetic factors that could be contributing to your overall cardiometabolic health (the health of your heart, blood vessels, and metabolic system).
By staying up to date on the latest findings in medical science and managing your risk factors, you may be able to avoid certain diseases and live a longer, healthier life.
AT NO COST
The Heart & Kidney Health Connection
When it comes to health, the kidneys work hand-in-hand with your heart. As your heart pumps oxygen-rich blood, your kidneys step in to clean it, removing waste and excess water. Their collaboration extends to controlling blood pressure, supporting bone health, producing red blood cells, and maintaining mineral balance.
Shared Risk Factors:
Heart and kidney disease also share common risk factors like diabetes, high cholesterol, and high blood pressure. Recognizing these shared risks emphasizes the importance of a big-picture approach to wellness, focusing on both heart and kidney health.
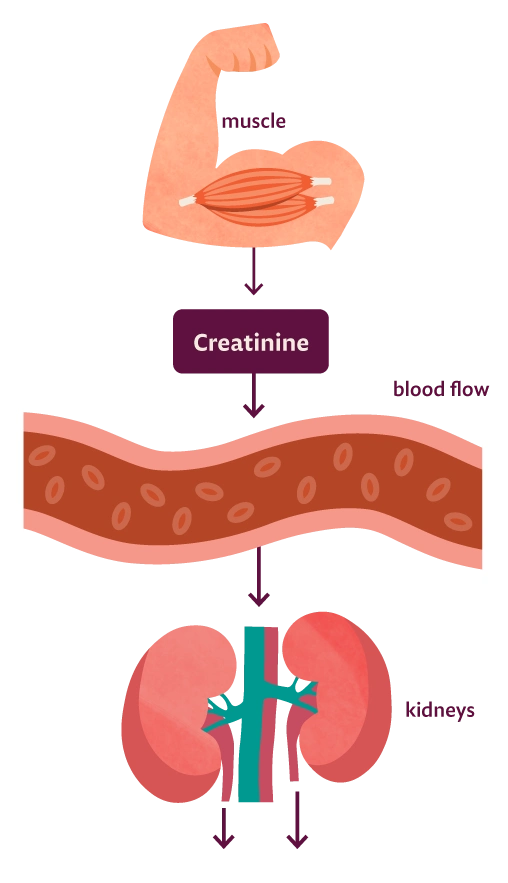
Measuring Kidney Health
To determine kidney health, your healthcare team might start with a creatinine test to check how well your kidneys are filtering this normal waste product from your blood. Your creatinine levels, together with your age and gender, determine your estimated glomerular filtration rate (eGFR). A normal eGFR indicates healthy kidney function, while a reduced eGFR may signal kidney disease. A decreased eGFR is also associated with an increased risk of cardiovascular events.
Monitoring kidney health is crucial, especially for individuals with shared risk factors like diabetes, high cholesterol, and high blood pressure. Regular assessments contribute to early detection and proactive management of both kidney and heart health.
Blood Sugar
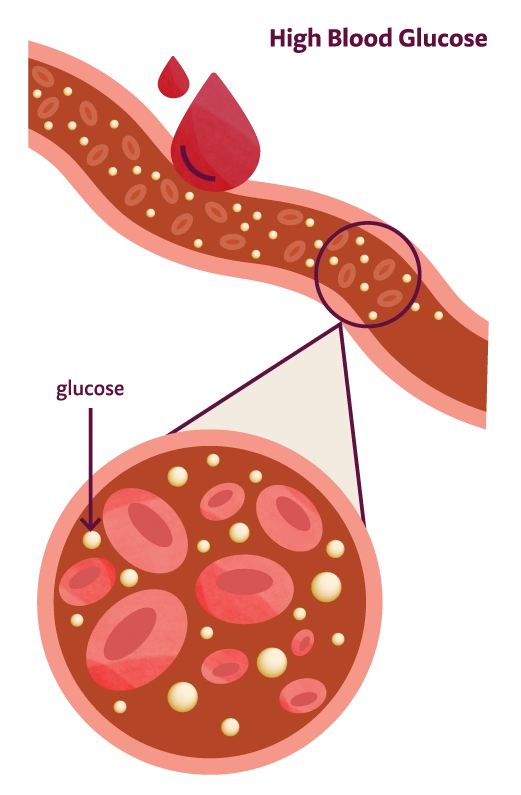
When you eat, your body turns the food into sugar (or glucose) that circulates in your bloodstream. As your blood sugar levels go up, this signals your body to release insulin, a hormone which breaks down the sugar so your body can use it as energy.
Your body usually keeps blood sugar levels in your body balanced. This balance is really important for your health. If your blood sugar level stays high for too long, it can lead to health problems like diabetes.
Diabetes is a chronic condition where you have too much sugar in your bloodstream. If you have diabetes, your body either doesn’t make enough insulin as the cells in your body don’t respond to insulin as they should, resulting in dangerously high glucose levels
There are different types of diabetes:
Why High Blood Glucose is Bad for Cardiometabolic Health
While we know that high blood glucose can lead to diabetes, we also know it can disrupt the normal function of your body. Here are a few ways that high blood glucose can affect your overall cardiometabolic health:
- Leads to diabetes
- Damages blood vessels
- Narrows arteries
- Increases blood pressure
- Causes cholesterol to build up
- Triggers inflammation
- Causes clotting which can lead to heart attacks and stroke
If you are concerned about diabetes or prediabetes, the American Diabetes Association has some additional resources.
Type 1 Diabetes
Type 1 diabetes is thought to be caused by an autoimmune reaction that stops your body from making insulin. This is the diabetes that kids sometimes have. Scientists are still learning about this type of diabetes, but currently no one knows how to prevent type 1 diabetes. If you do have it, it means you will need to inject insulin every day to manage your sugar levels.
Type 2 Diabetes
Type 2 diabetes is a more common type of diabetes, found in 90-95% of those who have diabetes. This is typically seen in adults. It develops over many years, & this type of diabetes is impacted by your weight, your diet, and your level of activity. The symptoms of type 2 diabetes are not always noticeable, so it is important to test blood sugar regularly.
Prediabetes
The term “prediabetic” does not mean you have diabetes, it means that your blood sugar is higher than normal, and you have a higher risk of developing type 2 diabetes. In the US, more than a third of the population has prediabetes and 80% of those people don’t know it.

Measuring Blood Sugar via A1c Lab Test
The A1c test, which is also called a Hemoglobin A1c or HbA1c test, is a blood test that measures the average blood sugar levels in your body over the past 2-3 months. The A1c test measures the percentage of your red blood cells that have sugar-coated hemoglobin (hemoglobin is the molecule in red blood cells that carries oxygen). While some percentage is perfectly normal, elevated numbers indicate prediabetes or diabetes. The CDC recommends that people who are overweight or who have other risk factors for diabetes, as well as all adults over 45 years old, get a baseline A1c test. Some factors like kidney disease, liver disease, severe anemia, and pregnancy can falsely affect your A1c, so speak with your doctor if you have abnormal results.
How to interpret your A1c test results:
Normal
Below 5.7%
Prediabetes
5.7% to 6.4%
Diabetes
6.5% or above
Source: Centers for Disease Control and Prevention (CDC)

Cholesterol
Cholesterol is a waxy, fat-like substance that our bodies need to survive and grow. It is a central building block for the cells in our body and it fulfills other important roles in the body. Cholesterol comes from two sources: 1) our bodies make it, and 2) we get it from the foods we eat.
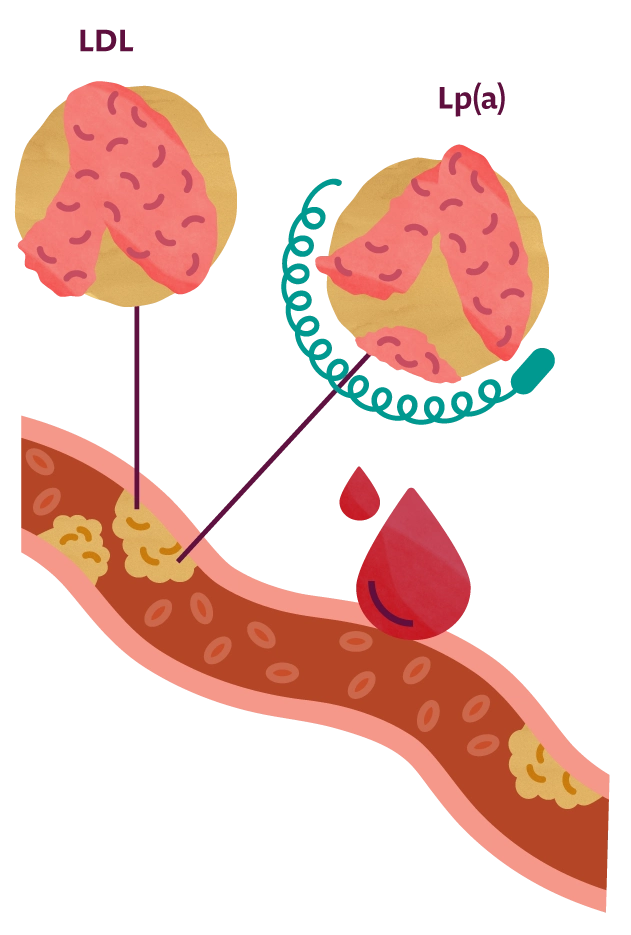
You’ve probably heard of LDL cholesterol, HDL cholesterol, and Triglycerides as types of lipids that your doctor checks when you get blood work completed. More recently, doctors are exploring new particles in the human body like Lp(a) and Apo B to get a more complete picture of your cardiometabolic health. However, let’s start with the basics before we explore these new types of cholesterol.
The Basics of Cholesterol:
LDL cholesterol
Low-density lipoprotein, or LDL, sometimes referred to as “bad” cholesterol, can lead to build-up in our arteries making us more likely to have a heart attack or a stroke.
HDL cholesterol
High-density lipoprotein, or HDL, is thought of as the “good” cholesterol because it carries LDL cholesterol away from the arteries to the liver where the LDL is processed and removed from the body.
Total cholesterol
Both LDL and HDL combined into one score.
Triglycerides
These are not cholesterol, but another type of lipid (or fat) in the blood. They store extra energy from the food we eat. Doctors believe that high levels of triglycerides are linked with increased cardiometabolic risk.
New Frontiers in Cholesterol
Apo B
Apolipoprotein B, or Apo B, carries bad cholesterol (LDL and VLDL) to where it needs to go in the body. When scientists find Apo B in the blood, it tells them that there's bad cholesterol present.
What's interesting is that each Apo B molecule is responsible for transporting exactly one piece of bad cholesterol. This makes it easy for scientists to count and measure how much bad cholesterol is in the blood accurately. In comparison, regular cholesterol tests estimate bad cholesterol by subtracting good cholesterol (HDL) from the total cholesterol, a measure which may not be very accurate for some people.
Because Apo B gives a more direct and reliable measure of the harmful cholesterol in the blood, doctors think that Apo B could be a better way to predict heart health.
Lp(a)
Lipoprotein(a), or Lp(a), is a type of cholesterol that is similar to the “bad” LDL cholesterol but even stickier. It consists of an LDL cholesterol particle with an extra protein attached to it called apolipoprotein(a).
LDL + the sticky apolipoprotein(a) protein = Lp(a).
Elevated levels of Lp(a) in your blood can contribute to blocked arteries, thus reducing blood flow to your heart, brain, and other vital organs. It can also increase clotting and can cause inflammation in blood vessels.
Facts about Lp(a):
- The level of Lp(a) you have in your body is mainly genetic, meaning it is inherited from your parents.
- 1 in 5 of us has a high level of Lp(a).
- Lp(a) levels in the Black population, on average, are more than 2x higher than in the White and Hispanic populations.
- High Lp(a) increases risk of heart attack at an early age by 3x. 1.
- Most people who have high Lp(a) are unaware.
- Conventional cholesterol tests don’t measure Lp(a), and most doctors do not routinely check Lp(a) when ordering blood tests.
- There is no drug currently available to lower Lp(a). Statins do not lower levels.
- Diet, exercise, and other lifestyle changes do not typically impact Lp(a) levels.
- Doctors are testing new medicines for lowering Lp(a) in an effort to decrease heart attacks and strokes.
What Can You Do About Lp(a)?
Lp(a) levels are just one part of your overall risk for cardiovascular disease. It’s important to talk to your doctor about your overall cardiovascular health including other risk factors to get a full understanding of your health. Knowing your level can help you better manage your overall risk.
Here are some steps you can take:
1. Get Tested
Ask your doctor to measure your Lp(a). This is especially important if you have cardiovascular disease including poor circulation in your legs, previous heart attack, stroke, or blocked arteries. It is also important to know your Lp(a) if you have a family member who has had a heart attack or stroke, or if you have other risk factors for cardiovascular disease. An Lp(a) test is included in our no-cost heart and kidney screening.
2. Manage Other Risk Factors
Lifestyle choices like eating a heart-healthy diet, getting regular exercise, and quitting smoking (if you smoke) are within your control. Your doctor can also advise you on medication to manage your blood sugar, cholesterol, and blood pressure if needed.
3. Get Involved in Studies for Investigational Lp(a) Treatments
Doctors and scientists are working together to find new medicines that will help lower Lp(a) levels. Seeing if you qualify for one of these studies could be a good way for you to have access to early investigational treatments while helping to make these new treatments available to others in the future. More on Lp(a).
4. Talk to Your Family & Friends
Lp(a) is primarily inherited, meaning if you have high Lp(a) your relatives, including your parents, siblings, and children, may also have the genetic risk factor. About 60 million Americans are estimated to have high Lp(a), meaning that one in five of us have it. Discuss Lp(a) with family and friends and encourage them to get screened.
Blood Pressure / High Blood Pressure
Your heart is constantly pumping blood into your organs. The force of that blood as it pushes against the walls of your arteries traveling from your heart to the rest of your body is measured as blood pressure. Your blood pressure goes up and down depending on what you are doing. “Hypertension” is a disease which is diagnosed when a person has persistent high blood pressure.
About half of American adults have high blood pressure. If that surprises you, you may also be surprised to learn that many people don’t know they have it, because most people with hypertension have NO symptoms. Which means it is important to check your blood pressure regularly.
Measuring Blood Pressure:
When it comes to blood pressure, there are two numbers you need to know:
- Systolic pressure - the top number which measures the pressure when your heart beats.
- Diastolic pressure - the bottom number which measures the pressure when your heart rests between beats.2
According to the American Heart Association, normal blood pressure is below 120 systolic, and below 80 diastolic, or less than 120/80 mm Hg. Measurements that are consistently higher than 120/80 suggest hypertension or high blood pressure.
The only way to know if you have high blood pressure is to measure it regularly. This can be done through your doctor, or at home with a blood pressure cuff.
Facts About High Blood Pressure: 3
- Generally doesn’t cause symptoms or warning signs
- Puts you at risk for heart disease, stroke, and kidney disease
- Is more common in Black adults (56%) than in White adults (48%)
- Affects a greater percentage of men (50%) than women (44%)

Why High Blood Pressure is a Concern
High blood pressure can damage your arteries by making them less elastic. This decreases the amount of blood and oxygen that goes to your heart causing things like chest pain, heart attack, and heart failure. It can also impact the arteries that supply blood to your brain and can increase your risk for a stroke or dementia later in life. Having high blood pressure, especially when it is combined with diabetes, also puts you at a much higher risk of developing chronic kidney disease.3
What Can You Do About High Blood Pressure?
1. Learn Your Levels
Since high blood pressure often has no symptoms, it is important to measure it either through your doctor or at home using a blood pressure cuff.
2. Manage Blood Glucose
Most people with diabetes also have high blood pressure. Getting your blood glucose under good control will also help reduce your risk for high blood pressure.
3. Take Your Medicine
Follow your doctor or health care professional’s instructions for medications to treat your blood pressure and other related conditions.
4. Manage Other Risk Factors
Lifestyle choices like eating a healthy diet, getting regular exercise, limiting alcohol, and quitting smoking (if you smoke), are also recommended.
Health-Related Behaviors

Smoking
Smoking is a major risk factor for heart disease and other cardiovascular problems. Chemicals in cigarette smoke cause your blood vessels to narrow which can lead to atherosclerosis (hardening of the arteries), coronary heart disease (disease of the heart arteries), stroke, and peripheral arterial disease (bad circulation in the legs). According to the Centers for Disease Control and Prevention (CDC), smokers who quit can significantly reduce the risk of disease and death from cardiovascular disease. 4

Diet
A healthy diet can reduce the risk of heart disease, stroke, and type 2 diabetes.5 The DASH diet which stands for Dietary Approaches to Stop Hypertension, is a flexible and balanced plan recommended by the National Heart Lung and Blood Institute. In studies, the DASH diet proved to be effective at lowering blood pressure, cholesterol, obesity, and the risk for developing type 2 diabetes and heart disease.6

Exercise
Being active can help you live longer and lower your risk of heart disease, type 2 diabetes, obesity, and even some cancers. Adults who get at least 150 minutes of moderate physical activity per week can lower their risk of heart disease and stroke. Those who don’t get this recommended amount of exercise but who do increase their physical activity, can start to see health benefits like lower blood pressure, lower triglycerides, and lower blood sugar.7 Check out the CDC recommendations on physical activities here.

Alcohol
The question of whether moderate alcohol drinking (on average 1 drink per day for women and 1-2 drinks per day for men) has some health benefits remains a topic of scientific interest and debate.8 On the other hand, doctors agree that there are many risks associated with heavy alcohol use. Excessive drinking can increase the risk of serious health problems including sudden death (for those with cardiovascular disease), cardiomyopathy (heart muscle weakness), stroke, high blood pressure, pancreatitis, and liver disease.9

Other Factors
The diseases and health conditions which run in your family can play a big role in your cardiometabolic health. You and your family share genes and you are likely to share common behaviors like your food and exercise habits.
If you have a family member with diabetes, you are more likely to develop it too. Heart disease and related conditions like high blood pressure and high cholesterol can also run in families. It is important to tell your doctor about your family health history, especially if your family members have had heart attacks or heart disease at a young age, as this may be a sign of a hereditary condition like high Lp(a) or familial hypercholesterolemia.10
Taking care of your weight is important for your overall health, especially as you get older. Having obesity, or significant excess weight, puts you at a much higher risk for many conditions and diseases including high blood pressure, high LDL cholesterol, high triglycerides, type 2 diabetes, heart disease, stroke, arthritic problems, and gallbladder disease. Healthy eating, exercise, sleep, and stress reduction all contribute to a healthy weight.11 Learn more about weight management.
Researchers have found that bad cardiometabolic health is more common among people who are non-white, male, poor, less educated, or older. This may be due to non-medical factors that influence their health.12 While these health disparities can be viewed through the lens of race and ethnicity, they go beyond that to include underserved communities such as the following:13
- Black, Latino, and other persons of color
- Those from religious minorities
- LGBTQ+ persons
- Persons with disabilities
- Those who live in rural areas
- People impacted by poverty or inequality
- Those with language barriers
According to the American Heart Association, our blood vessels lose elasticity as we get older, making us more likely to develop high blood pressure.14 People who are 65 and older are much more likely to have a heart attack, stroke, or develop heart disease.
Heart disease is the leading cause of death for both men and women, but there are interesting sex-related differences. Men often develop heart disease at a younger age than women. This difference is partly due to female sex hormones, which help maintain the health of blood vessels, at least until they go through menopause.
The area where cholesterol builds up in the body also varies based on your sex. In men, it typically accumulates in major arteries, while in women, it tends to affect smaller blood vessels.
Additionally, the location of body fat varies between the sexes. Women tend to store extra fat around their hips, thighs, and butt, whereas men tend to carry it in their bellies.15
Disclaimer
The information provided on Care Access is intended for informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Our products and content are not intended to diagnose, treat, cure, or prevent any disease.